Page 623 - Read Online
P. 623
Page 2 of 18 Wilgus. Plast Aesthet Res 2020;7:54 I http://dx.doi.org/10.20517/2347-9264.2020.150
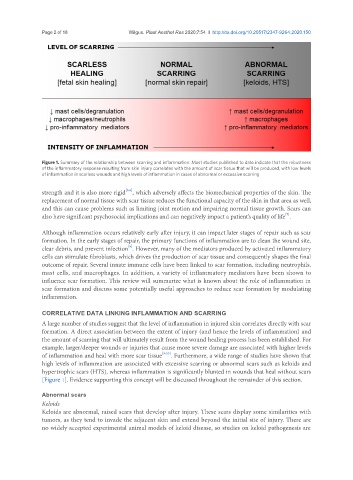
Figure 1. Summary of the relationship between scarring and inflammation. Most studies published to date indicate that the robustness
of the inflammatory response resulting from skin injury correlates with the amount of scar tissue that will be produced, with low levels
of inflammation in scarless wounds and high levels of inflammation in cases of abnormal or excessive scarring
[5,6]
strength and it is also more rigid , which adversely affects the biomechanical properties of the skin. The
replacement of normal tissue with scar tissue reduces the functional capacity of the skin in that area as well,
and this can cause problems such as limiting joint motion and impairing normal tissue growth. Scars can
[7]
also have significant psychosocial implications and can negatively impact a patient’s quality of life .
Although inflammation occurs relatively early after injury, it can impact later stages of repair such as scar
formation. In the early stages of repair, the primary functions of inflammation are to clean the wound site,
[8]
clear debris, and prevent infection . However, many of the mediators produced by activated inflammatory
cells can stimulate fibroblasts, which drives the production of scar tissue and consequently shapes the final
outcome of repair. Several innate immune cells have been linked to scar formation, including neutrophils,
mast cells, and macrophages. In addition, a variety of inflammatory mediators have been shown to
influence scar formation. This review will summarize what is known about the role of inflammation in
scar formation and discuss some potentially useful approaches to reduce scar formation by modulating
inflammation.
CORRELATIVE DATA LINKING INFLAMMATION AND SCARRING
A large number of studies suggest that the level of inflammation in injured skin correlates directly with scar
formation. A direct association between the extent of injury (and hence the levels of inflammation) and
the amount of scarring that will ultimately result from the wound healing process has been established. For
example, larger/deeper wounds or injuries that cause more severe damage are associated with higher levels
of inflammation and heal with more scar tissue [9-13] . Furthermore, a wide range of studies have shown that
high levels of inflammation are associated with excessive scarring or abnormal scars such as keloids and
hypertrophic scars (HTS), whereas inflammation is significantly blunted in wounds that heal without scars
[Figure 1]. Evidence supporting this concept will be discussed throughout the remainder of this section.
Abnormal scars
Keloids
Keloids are abnormal, raised scars that develop after injury. These scars display some similarities with
tumors, as they tend to invade the adjacent skin and extend beyond the initial site of injury. There are
no widely accepted experimental animal models of keloid disease, so studies on keloid pathogenesis are