Page 157 - Read Online
P. 157
Nardulli. Plast Aesthet Res 2020;7:15 I http://dx.doi.org/10.20517/2347-9264.2019.56 Page 7 of 10
A B
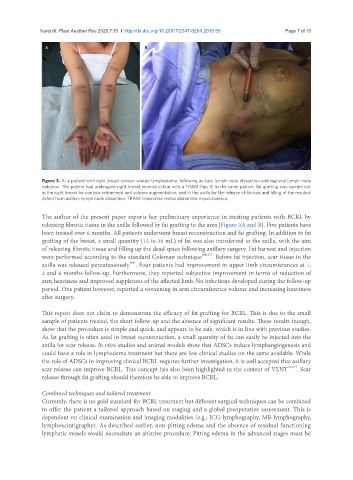
Figure 3. A: a patient with right breast cancer-related lymphedema, following axillary lymph node dissection and regional lymph node
radiation. The patient had undergone right breast reconstruction with a TRAM-flap; B: in the same patient, fat grafting was carried out
in the right breast for contour refinement and volume augmentation, and in the axilla for the release of fibrosis and filling of the residual
defect from axillary lymph node dissection. TRAM: transverse rectus abdominis myocutaneous
The author of the present paper reports her preliminary experience in treating patients with BCRL by
releasing fibrotic tissue in the axilla followed by fat grafting to the area [Figure 3A and B]. Five patients have
been treated over 6 months. All patients underwent breast reconstruction and fat grafting. In addition to fat
grafting of the breast, a small quantity (15 to 30 mL) of fat was also transferred to the axilla, with the aim
of releasing fibrotic tissue and filling up the dead space following axillary surgery. Fat harvest and injection
were performed according to the standard Coleman technique [46,47] . Before fat injection, scar tissue in the
[48]
axilla was released percutaneously . Four patients had improvement in upper limb circumferences at 1,
3 and 6 months follow-up. Furthermore, they reported subjective improvement in terms of reduction of
arm heaviness and improved suppleness of the affected limb. No infections developed during the follow-up
period. One patient however, reported a worsening in arm circumference volume and increasing heaviness
after surgery.
This report does not claim to demonstrate the efficacy of fat grafting for BCRL. This is due to the small
sample of patients treated, the short follow-up and the absence of significant results. These results though,
show that the procedure is simple and quick, and appears to be safe, which is in line with previous studies.
As fat grafting is often used in breast reconstruction, a small quantity of fat can easily be injected into the
axilla for scar release. In vitro studies and animal models show that ADSCs induce lymphangiogenesis and
could have a role in lymphedema treatment but there are few clinical studies on the same available. While
the role of ADSCs in improving clinical BCRL requires further investigation, it is well accepted that axillary
scar release can improve BCRL. This concept has also been highlighted in the context of VLNT [2,27] . Scar
release through fat grafting should therefore be able to improve BCRL.
Combined techniques and tailored treatment
Currently, there is no gold standard for BCRL treatment but different surgical techniques can be combined
to offer the patient a tailored approach based on staging and a global preoperative assessment. This is
dependent on clinical examination and imaging modalities (e.g., ICG-lymphography, MR-lymphography,
lymphoscintigraphy). As described earlier, non-pitting edema and the absence of residual functioning
lymphatic vessels would necessitate an ablative procedure. Pitting edema in the advanced stages must be