Page 74 - Read Online
P. 74
Funahashi et al. Mini-invasive Surg 2018;2:27 I http://dx.doi.org/10.20517/2574-1225.2018.28 Page 9 of 12
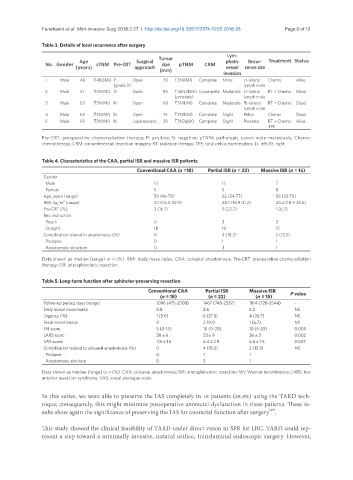
Table 3. Details of local recurrence after surgery
Lym-
Tumor
Age Surgical phatic Recur- Treatment Status
No. Gender cTNM Pre-CRT size pTNM CRM
(years) approach vessel rence site
(mm)
invasion
1 Male 46 T4N2M0 P Open 70 T3N0M0 Complete None Lt-lateral Chemo Alive
(grade 2) lymph node
2 Male 51 T3N1M0 N Open 85 T4bN2bM0 Incomplete Moderate Lt-lateral RT + Chemo Dead
(prostate) lymph node
3 Male 63 T3N1M0 N Open 60 T3N1bN0 Complete Moderate Rt-lateral RT + Chemo Dead
lymph node
4 Male 63 T3N1M0 N Open 75 T3N1bN0 Complete Slight Pelvis Chemo Dead
5 Male 59 T3N1M0 N Laparoscopic 20 T3N2aM0 Complete Slight Prostate RT + Chemo Alive
TPE
Pre-CRT: preoperative chemoradiation therapy; P: positive; N: negative; pTNM: pathologic tumor-node-metastasis; Chemo:
chemotherapy; CRM: circumferential resection margins; RT: radiation therapy; TPE: total pelvic exenteration; Lt: left; Rt: right
Table 4. Characteristics of the CAA, partial ISR and massive ISR patients
Conventional CAA (n =18) Partial ISR (n = 22) Massive ISR (n = 15)
Gender
Male 13 17 7
Female 5 5 8
Age, years (range) 59 (46-79) 62 (34-77) 56 (33-70)
2
BMI, kg/m (range) 22.1(16.5-32.9) 24.7 (16.9-31.2) 20.4 (18.3-26.5)
Pre-CRT (%) 3 (16.7) 5 (22.7) 1 (6.7)
Reconstruction
Pouch 0 3 3
Straight 18 19 12
Complication related to anastomosis (%) 0 4 (18.2) 2 (13.3)
Prolapse 0 1 1
Anastomotic structure 0 3 1
Data shown as median (range) or n (%). BMI: body mass index; CAA: coloanal anastomosis; Pre-CRT: preoperative chemoradiation
therapy; ISR: intersphincteric resection
Table 5. Long-term function after sphincter-preserving resection
Conventional CAA Partial ISR Massive ISR P value
(n = 18) (n = 22) (n = 15)
Follow-up period, days (range) 1096 (475-2508) 1467 (748-2537) 1814 (728-2544) -
Daily bowel movements 0.8 2.6 2.2 NS
Urgency (%) 1 (5.6) 6 (27.3) 4 (26.7) NS
Fecal incontinence 0 2 (9.1) 1 (6.7) NS
WI score 5 (0-14) 10 (0-20) 10 (5-20) 0.005
LARS score 28 ± 6 33 ± 9 36 ± 3 0.002
VAS score 7.8 ± 1.5 6.4 ± 2.9 6.6 ± 1.5 0.047
Complication related to coloanal anastomosis (%) 0 4 (18.2) 2 (13.3) NS
Prolapse 0 1 1
Anastomotic stricture 0 3 1
Data shown as median (range) or n (%). CAA: coloanal anastomosis; ISR: intersphincteric resection; WI: Wexner incontinence; LARS: low
anterior resection syndrome; VAS: visual analogue scale
In this series, we were able to preserve the IAS completely in 18 patients (28.8%) using the TARD tech-
nique; consequently, this might minimize postoperative anorectal dysfunction in these patients. These re-
[49]
sults show again the significance of preserving the IAS for anorectal function after surgery .
This study showed the clinical feasibility of TARD under direct vision in SPR for LRC. TARD could rep-
resent a step toward a minimally invasive, natural orifice, transluminal endoscopic surgery. However,