Page 64 - Read Online
P. 64
de Kouchkovsky et al. J Transl Genet Genom 2021;5:265-77 https://dx.doi.org/10.20517/jtgg.2021.32 Page 269
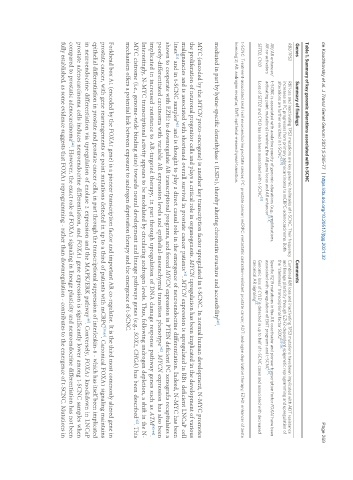
Table 1. Summary of key genomic alterations associated with t-SCNC
Genes Summary of findings Comments
RB1/TP53 RB1 loss and inactivating TP53 mutations are key genomic hallmarks of t-SCNC. Their frequency Combined RB1 loss and inactivating TP53 mutations have been implicated with ADT resistance
increases as PC progresses from primary adenocarcinoma to mCRPC-adenocarcinoma. Both and lineage plasticity through EZH2-dependent epigenetic reprogramming and upregulation of
[3,11] [23-26]
alterations are further enriched in t-SCNC the “stemness” transcriptional factor SOX2
AR/AR enhancer/ t-SCNC is associated with a relative paucity of genomic alterations (e.g., amplifications, Specific R219 mutations in the AR coactivator and pioneer transcription factor FOXA1 have been
[3,14] [30]
AR co-activators activating point mutations) involving the AR gene locus and AR enhancer associated with upregulation of EMT programs and t-SCNC
SETD2, CYLD Loss of SETD2 and CYLD has also been associated with t-SCNC [3] Genomic loss of CYLD is detected in up to half of t-SCNC cases and associated with decreased
[3]
canonical AR signaling
t-SCNC: Treatment-associated small cell neuroendocrine prostate cancer; PC: prostate cancer; mCRPC: metastatic castration-resistant prostate cancer; ADT: androgen deprivation therapy; EZH2: enhancer of zeste
homolog 2; AR: androgen receptor; EMT: epithelial-mesenchymal-transition.
[40]
mediated in part by lysine-specific demethylase 1 (LSD1), thereby altering chromatin structure and accessibility .
MYC (encoded by the MYCN proto-oncogene) is another key transcription factor upregulated in t-SCNC. In normal human development, N-MYC promotes
the proliferation of neuronal progenitor cells and plays a critical role in organogenesis. MYCN upregulation has been implicated in the development of various
malignancies and is associated with shortened overall survival in prostate cancer patients . MYCN expression is upregulated in RB1 deficient LNCaP cell
[41]
lines and in t-SCNC samples and is thought to play a direct causal role in the emergence of neuroendocrine differentiation. Indeed, N-MYC has been
[42]
[21]
shown to cooperate with EZH2 to downregulate AR transcriptional programs, and forced MYCN expression in PTEN deficient PC xenografts recapitulates a
poorly-differentiated carcinoma with variable AR expression levels and epithelial-mesenchymal transition phenotype . MYCN expression has also been
[42]
implicated in increased resistance to AR-targeted therapy, in part through upregulation of DNA damage response pathway genes such as ATM [42-44] .
Interestingly, N-MYC transcriptional activity appears to be modulated by circulating androgen levels. Thus, following androgen depletion, a shift in the N-
MYC cistrome (i.e., genome-wide binding sites) towards neural development and lineage pathways genes (e.g., SOX2, CHGA) has been described . This
[42]
mechanism offers a potential link between exposure to androgen deprivation therapy and the emergence of t-SCNC.
Forkhead box A1 (encoded by the FOXA1 gene) is a pioneer transcription factor and important AR co-regulator. It is the third most commonly altered gene in
prostate cancer, with gene rearrangements or point mutations detected in up to a third of patients with mCRPC [30,45] . Canonical FOXA1 signaling maintains
epithelial differentiation in prostate and prostate cancer cells, in part through the transcriptional suppression of interleukin-8 - which has itself been implicated
[46]
in neuroendocrine differentiation via upregulation of enolase 2 expression and the MAPK/ERK pathway . Conversely, FOXA1 knockdown in LNCaP
prostate adenocarcinoma cells induces neuroendocrine differentiation, and FOXA1 gene expression is significantly lower among t-SCNC samples when
compared to prostatic adenocarcinoma . However, the exact role of FOXA1 signaling in lineage plasticity and neuroendocrine differentiation has not been
[46]
fully established, as some evidence suggests that FOXA1 reprogramming - rather than downregulation - contributes to the emergence of t-SCNC. Mutations in