Page 10 - Read Online
P. 10
Page 4 of 9 Tyerman et al. J Cancer Metastasis Treat 2022;8:29 https://dx.doi.org/10.20517/2394-4722.2022.20
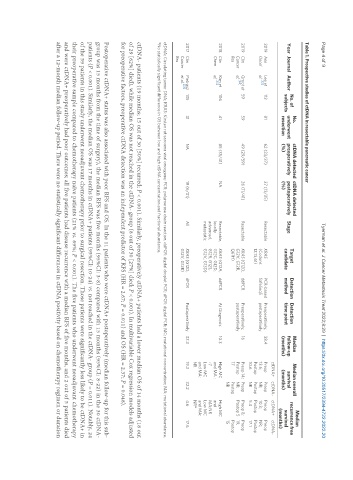
Table 1. Prospective studies of ctDNA in resectable pancreatic cancer
Median
No. ctDNA detected ctDNA detected Median Median overall
Year Journal Author No. of underwent preoperatively postoperatively Stage Target Detection Detection follow-up survival recurrence free
time point
method
candidate
subjects
survival
resection (%) (%) (months) (months)
(months)
ctDNA+ ctDNA- ctDNA+ ctDNA-
2019 Ann Lee et 112 81 62 (23/37) 37 (13/35) Resectable KRAS PCR-based Preoperatively, 38.4 Preop Preop Preop Preop
[32]
Oncol al. (Codons SafeSeqS postoperatively 13.6; NR; 10.3; NR;
12,13,61) Postop Postop Postop Postop
10.6 NR 5.4 17.1
2019 Clin Groot et 59 59 49 (29/59) 26 (11/41) Resectable KRAS (G12D, ddPCR Preoperatively, 16 Preop 14; Preop Preop 8; Preop
[34]
Cancer al. G12V, G12R, postoperatively Postop NR; Postop 5 19;
Res Q61H) 17 Postop Postop
NR 15
2018 Clin Kim et 106 41 85 (35/41) NA Resectable, KRAS (G12A, ddPCR At Diagnosis 10.3 High MC High MC
[35]
Chem al. locally G12C, G12D, and MA : and
advanced, G12R, G12S, ~7 MA:NR
metastatic G12V, G13D) Low MC Low MC
and MA: and MA:
NR NR*
2017 Clin Pietrasz 135 31 NA 19 (6/31) All KRAS (G12D, dPCR Postoperatively 33.3 19.3 32.2 4.6 17.6
Cancer et al. [33] G12V, G12R)
Res
ctDNA: Circulating tumor DNA; KRAS: Kirsten rat sarcoma viral oncogene; PCR: polymerase chain reaction. ddPCR: digital droplet PCR; dPCR: digital PCR; MC: mutational concentration; MA: mutational abundance.
*No statistically significant difference in OS between low and high ctDNA concentration and fractional abundance.
ctDNA- patients (19 months; 15 out of 30 [50%] recurred; P < 0.001). Similarly, preoperatively ctDNA+ patients had a lower median OS of 14 months (18 out
of 29 [62%] died), while median OS was not reached in the ctDNA- group (8 out of 30 [27%] died; P < 0.001). In multivariable Cox regression models adjusted
for preoperative factors, preoperative ctDNA detection was an independent predictor of RFS (HR = 2.67; P = 0.011) and OS (HR = 2.37; P = 0.048).
Postoperative ctDNA+ status was also associated with poor RFS and OS. In the 11 patients who were ctDNA+ postoperatively (median follow-up for this sub-
group was 15 months from the time of surgery), the median RFS was five months (95%CI: 3-8) compared with 15 months (95%CI: 8-22) in the 30 ctDNA-
patients (P < 0.001). Similarly, the median OS was 17 months in ctDNA+ patients (95%CI: 10-24) vs. not reached in the ctDNA- group (P = 0.011). Notably, 24
of the 59 patients in this study underwent neoadjuvant chemotherapy prior to surgical resection. Those patients were significantly less likely to be ctDNA+ in
their preoperative sample compared to chemotherapy naïve patients (21% vs. 69%; P < 0.001). The five patients who underwent neoadjuvant chemotherapy
and were ctDNA+ preoperatively had poor outcomes; all five patients had disease recurrence with a median RFS of five months, and 2 out of 5 patients died
after a 12-month median follow-up period. There were no statistically significant differences in ctDNA positivity based on chemotherapy regimen or duration