Page 106 - Read Online
P. 106
Kotecha et al. J Cancer Metastasis Treat 2021;7:67 https://dx.doi.org/10.20517/2394-4722.2021.163 Page 3 of 11
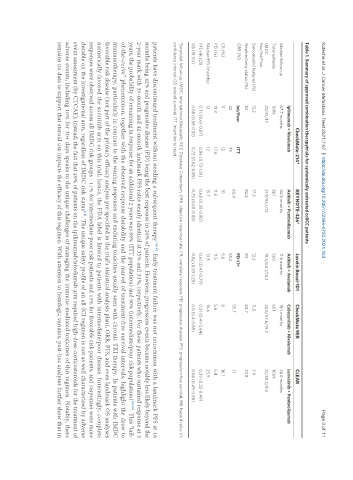
Table 1. Summary of approved combination therapytrials for systemically untreated ccRCC patients
CheckMate-214* KEYNOTE-426* Javelin Renal-101 CheckMate 9ER CLEAR
Ipilimumab + Nivolumab Axitinib + Pembrolizumab Axitinib + Avelumab Cabozantinib + Nivolumab Lenvatinib + Pembrolizumab
Median follow-up 67.7 months 42.8 months 11.6 months 18.1 months 26.6 months
Total patients 1096 861 560 651 1069
IMDC 23/61/17 31.9/55.1/13 19.3/64.1/16.3 22.6/57.6/19.7 31/59.2/9.3
Fav/Int/Poor
Sarcomatoid features (%) 13.2 17.9 12.2 11.5 7.9
Nephrectomy status (%) 82 82.6 83 68.7 73.8
ORR (%) Int/Poor ITT PD-L1+
60.4 55.7 71
42 39 55.2
CR (%) 11 12 10 5.6 8 16.1
PD (%) 19.3 17.6 11.3 11.5 5.6 5.4
Median PFS (months) 12 12 15.7 13.8 16.6 23.9
PFS HR (CI) 0.73 (0.61-0.87) 0.86 (0.73-1.01) 0.68 (0.58-0.80) 0.61 (0.47-0.79) 0.51 (0.41-0.64) 0.39 (0.32-0.49)
OS HR (CI) 0.68 (0.58-0.81) 0.72 (0.62-0.85) 0.73 (0.60-0.88) 0.82 (0.53-1.28) 0.6 (0.4-0.89) 0.66 (0.49-0.88)
*Extended follow-up. IMDC: International Metastatic RCC Database Consortium; ORR: objective response rate; CR: complete response; PD: progressive disease; PFS: progression-free survival; HR: hazard ratio; CI:
confidence interval; OS: overall survival; ITT: intention to treat.
patients have discontinued treatment without needing a subsequent therapy [18,19] . Early treatment failure was not uncommon with a landmark PFS at 18
months being 42% and progressive disease (PD) being the best response in 20% of patients. However, progression events became notably less likely beyond the
2-year mark with 30-month and 42-month landmark PFS rates nearly identical at 35% and 33%, respectively. For those patients who sustained response at 3
years, the probability of remaining in response for an additional 2 years was 89% (ITT population) and 90% (intermediate/poor risk population) [18,19] . This “tail-
of-the-curve” phenomenon, together with the observed response durability and the marvel of treatment-free survival intervals, highlight the draw to
immunotherapy, particularly in contrast to the waning responses and enduring toxicities usually seen with chronic TKI therapy. In patients with IMDC
favorable risk disease (not part of the primary efficacy analysis pre-specified in the trial’s statistical analysis plan), ORR, PFS, and even landmark OS analyses
numerically favored the sunitinib arm on this trial; hence, the FDA label is limited to patients with intermediate/poor disease. Interestingly, complete
responses were observed across all IMDC risk groups - 11% for intermediate-poor risk patients and 13% for favorable risk patients, and responses were more
durable on the investigational arm, regardless of IMDC risk status . The unique safety profile of an all-ICI regimen is not as well characterized by adverse
[18]
event assessment (by CTCAE); instead, the fact that 29% of patients on the ipilimumab/nivolumab arm required high-dose corticosteroids for the treatment of
adverse events, including 10% for 30+ days speaks to the unique challenges of managing the immune-mediated toxicities of this regimen. Notably, there
remains no data to support that steroid use impacts the efficacy of this regimen. With attention to histologic variants, post-hoc analyses further show that in