Page 120 - Read Online
P. 120
Bose et al. Hepatoma Res 2019;5:24 I http://dx.doi.org/10.20517/2394-5079.2019.10 Page 3 of 9
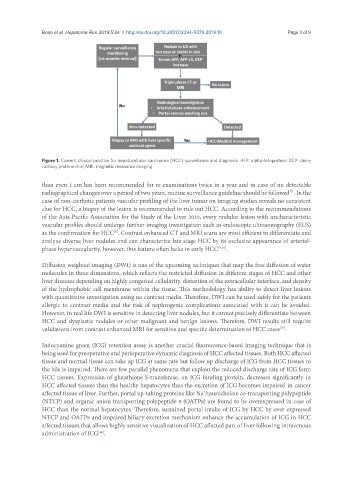
Figure 1. Current clinical practice for hepatocellular carcinoma (HCC) surveillance and diagnosis. AFP: alpha-fetoprotein; DCP: des-γ
carboxy prothrombin; MRI: magnetic resonance imaging
than even 1 cm has been recommended for re-examinations twice in a year and in case of no detectable
radiographical changes over a period of two years, routine surveillance guideline should be followed . In the
[7]
case of non-cirrhotic patients vascular profiling of the liver tumor on imaging studies reveals no consistent
clue for HCC, a biopsy of the lesion is recommended to rule out HCC. According to the recommendations
of the Asia-Pacific Association for the Study of the Liver 2010, every nodular lesion with uncharacteristic
vascular profiles should undergo further imaging investigation such as endoscopic ultrasonography (EUS)
as the confirmation for HCC . Contrast enhanced CT and MRI scans are most efficient in differentiate and
[8]
analyze diverse liver nodules and can characterize late stage HCC by its exclusive appearance of arterial-
phase hypervascularity, however, this feature often lacks in early HCC [9,10] .
Diffusion weighted imaging (DWI) is one of the upcoming techniques that map the free diffusion of water
molecules in three dimensions, which reflects the restricted diffusion in different stages of HCC and other
liver diseases depending on highly congested cellularity, distortion of the extracellular interface, and density
of the hydrophobic cell membrane within the tissue. This methodology has ability to detect liver lesions
with quantitative investigation using no contrast media. Therefore, DWI can be used safely for the patients
allergic to contrast media and the risk of nephrogenic complications associated with it can be avoided.
However, in real life DWI is sensitive in detecting liver nodules, but it cannot precisely differentiate between
HCC and dysplastic nodules or other malignant and benign lesions. Therefore, DWI results still require
validations from contrast enhanced MRI for sensitive and specific determination of HCC cases .
[11]
Indocyanine green (ICG) retention assay is another crucial fluorescence-based imaging technique that is
being used for preoperative and perioperative dynamic diagnosis of HCC affected tissues. Both HCC affected
tissue and normal tissue can take up ICG at same rate but follow up discharge of ICG from HCC tissues to
the bile is impaired. There are few parallel phenomena that explain the reduced discharge rate of ICG form
HCC tissues. Expression of glutathione S-transferase, an ICG binding protein, decreases significantly in
HCC affected tissues than the healthy hepatocytes thus the excretion of ICG becomes impaired in cancer
affected tissue of liver. Further, portal up-taking proteins like Na /taurocholate co-transporting polypeptide
+
(NTCP) and organic anion transporting polypeptide 8 (OATP8) are found to be overexpressed in case of
HCC than the normal hepatocytes. Therefore, sustained portal intake of ICG by HCC by over expressed
NTCP and OATP8 and impaired biliary excretion mechanism enhance the accumulation of ICG in HCC
affected tissues that allows highly sensitive visualization of HCC affected part of liver following intravenous
administration of ICG .
[12]