Page 37 - Read Online
P. 37
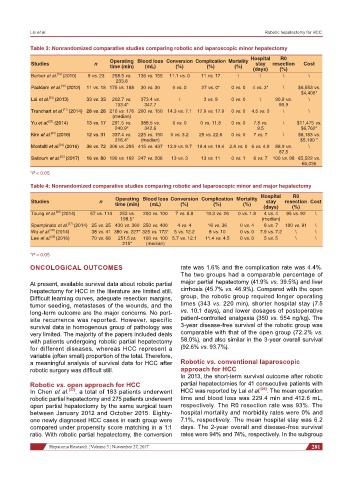
Lai et al. Robotic hepatectomy for HCC
Table 3: Nonrandomized comparative studies comparing robotic and laparoscopic minor hepatectomy
Hospital R0
Studies n Operating Blood loss Conversion Complication Mortality stay resection Cost
time (min) (mL) (%) (%) (%) (days) (%)
[18]
Berber et al. (2010) 9 vs. 23 258.5 vs. 136 vs. 155 11.1 vs. 0 11 vs. 17 \ \ \ \
233.6
[19]
Packiam et al. (2012) 11 vs. 18 175 vs. 188 30 vs. 30 0 vs. 0 27 vs. 0* 0 vs. 0 4 vs. 3* \ $6,553 vs.
$4,408*
[20]
Lai et al. (2013) 33 vs. 33 202.7 vs. 373.4 vs. \ 3 vs. 9 0 vs. 0 \ 90.9 vs. \
133.4* 347.7 90.9
[21]
Tranchart et al. (2014) 28 vs. 28 210 vs. 176 200 vs. 150 14.3 vs. 7.1 17.9 vs. 17.9 0 vs. 0 4.5 vs. 3 \ \
(median)
[22]
Yu et al. (2014) 13 vs. 17 291.5 vs. 388.5 vs. 0 vs. 0 0 vs. 11.8 0 vs. 0 7.8 vs. \ $11,475 vs.
240.9* 342.6 9.5 $6,762*
[23]
Kim et al. (2016) 12 vs. 31 337.4 vs. 225 vs. 150 0 vs. 3.2 25 vs. 22.6 0 vs. 0 7 vs. 7 \ $8,183 vs.
216.4* (median) $5,190 *
[24]
Montalti et al. (2016) 36 vs. 72 306 vs. 295 415 vs. 437 13.9 vs. 9.7 19.4 vs. 19.4 2.8 vs. 0 6 vs. 4.9 88.9 vs. \
87.5
[25]
Salloum et al. (2017) 16 vs. 80 190 vs. 162 247 vs. 206 13 vs. 3 13 vs. 11 0 vs. 1 6 vs. 7 100 vs. 98 €5,522 vs.
€6,035
*P < 0.05
Table 4: Nonrandomized comparative studies comparing robotic and laparoscopic minor and major hepatectomy
Operating Blood loss Conversion Complication Mortality Hospital R0
Studies n stay resection Cost
time (min) (mL) (%) (%) (%) (days) (%)
[26]
Tsung et al. (2014) 57 vs. 114 253 vs. 200 vs. 100 7 vs. 8.8 19.3 vs. 26 0 vs. 1.8 4 vs. 4 95 vs. 92 \
198.5* (median)
Spampinato et al. (2014) 25 vs. 25 430 vs. 360 250 vs. 400 4 vs. 4 16 vs. 36 0 vs. 4 8 vs. 7 100 vs. 91 \
[27]
Wu et al. (2014) 38 vs. 41 380 vs. 227* 325 vs. 173* 5 vs. 12.2 8 vs. 10 0 vs. 0 7.9 vs. 7.2 \ \
[28]
Lee et al. [29] (2016) 70 vs. 66 251.5 vs. 100 vs. 100 5.7 vs. 12.1 11.4 vs. 4.5 0 vs. 0 5 vs. 5 \ \
215* (median)
*P < 0.05
ONCOLOGICAL OUTCOMES rate was 1.6% and the complication rate was 4.4%.
The two groups had a comparable percentage of
At present, available survival data about robotic partial major partial hepatectomy (41.9% vs. 39.5%) and liver
hepatectomy for HCC in the literature are limited still. cirrhosis (45.7% vs. 46.9%). Compared with the open
Difficult learning curves, adequate resection margins, group, the robotic group required longer operating
tumor seeding, metastases of the wounds, and the times (343 vs. 220 min), shorter hospital stay (7.5
long-term outcome are the major concerns. No port- vs. 10.1 days), and lower dosages of postoperative
site recurrence was reported. However, specific patient-controlled analgesia (350 vs. 554 ng/kg). The
survival data in homogenous group of pathology was 3-year disease-free survival of the robotic group was
very limited. The majority of the papers included deals comparable with that of the open group (72.2% vs.
with patients undergoing robotic partial hepatectomy 58.0%), and also similar in the 3-year overall survival
for different diseases, whereas HCC represent a (92.6% vs. 93.7%).
variable (often small) proportion of the total. Therefore,
a meaningful analysis of survival data for HCC after Robotic vs. conventional laparoscopic
robotic surgery was difficult still. approach for HCC
In 2013, the short-term survival outcome after robotic
Robotic vs. open approach for HCC partial hepatectomies for 41 consecutive patients with
In Chen et al. [33] , a total of 183 patients underwent HCC was reported by Lai et al. [20] . The mean operation
robotic partial hepatectomy and 275 patients underwent time and blood loss was 229.4 min and 412.6 mL,
open partial hepatectomy by the same surgical team respectively. The R0 resection rate was 93%. The
between January 2012 and October 2015. Eighty- hospital mortality and morbidity rates were 0% and
one newly diagnosed HCC cases in each group were 7.1%, respectively. The mean hospital stay was 6.2
compared under propensity score matching in a 1:1 days. The 2-year overall and disease-free survival
ratio. With robotic partial hepatectomy, the conversion rates were 94% and 74%, respectively. In the subgroup
Hepatoma Research ¦ Volume 3 ¦ November 27, 2017 281