Page 21 - Read Online
P. 21
Chok Surgical strategy for huge/advanced HCC
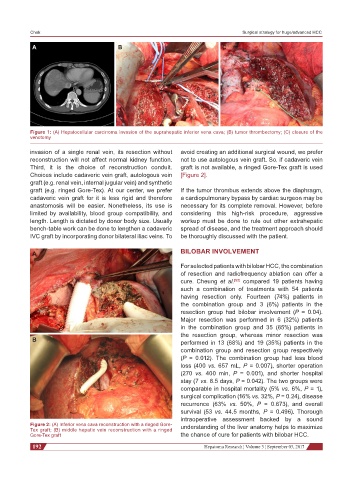
A B C
Figure 1: (A) Hepatocellular carcinoma invasion of the suprahepatic inferior vena cava; (B) tumor thrombectomy; (C) closure of the
venotomy
invasion of a single renal vein, its resection without avoid creating an additional surgical wound, we prefer
reconstruction will not affect normal kidney function. not to use autologous vein graft. So, if cadaveric vein
Third, it is the choice of reconstruction conduit. graft is not available, a ringed Gore-Tex graft is used
Choices include cadaveric vein graft, autologous vein [Figure 2].
graft (e.g. renal vein, internal jugular vein) and synthetic
graft (e.g. ringed Gore-Tex). At our center, we prefer If the tumor thrombus extends above the diaphragm,
cadaveric vein graft for it is less rigid and therefore a cardiopulmonary bypass by cardiac surgeon may be
anastomosis will be easier. Nonetheless, its use is necessary for its complete removal. However, before
limited by availability, blood group compatibility, and considering this high-risk procedure, aggressive
length. Length is dictated by donor body size. Usually workup must be done to rule out other extrahepatic
bench-table work can be done to lengthen a cadaveric spread of disease, and the treatment approach should
IVC graft by incorporating donor bilateral iliac veins. To be thoroughly discussed with the patient.
A BILOBAR INVOLVEMENT
For selected patients with bilobar HCC, the combination
of resection and radiofrequency ablation can offer a
cure. Cheung et al. [52] compared 19 patients having
such a combination of treatments with 54 patients
having resection only. Fourteen (74%) patients in
the combination group and 3 (6%) patients in the
resection group had bilobar involvement (P = 0.04).
Major resection was performed in 6 (32%) patients
in the combination group and 35 (65%) patients in
the resection group, whereas minor resection was
B performed in 13 (68%) and 19 (35%) patients in the
combination group and resection group respectively
(P = 0.012). The combination group had less blood
loss (400 vs. 657 mL, P = 0.007), shorter operation
(270 vs. 400 min, P = 0.001), and shorter hospital
stay (7 vs. 8.5 days, P = 0.042). The two groups were
comparable in hospital mortality (5% vs. 6%, P = 1),
surgical complication (16% vs. 32%, P = 0.24), disease
recurrence (63% vs. 50%, P = 0.673), and overall
survival (53 vs. 44.5 months, P = 0.496). Thorough
intraoperative assessment backed by a sound
Figure 2: (A) Inferior vena cava reconstruction with a ringed Gore- understanding of the liver anatomy helps to maximize
Tex graft; (B) middle hepatic vein reconstruction with a ringed
Gore-Tex graft the chance of cure for patients with bilobar HCC.
192 Hepatoma Research ¦ Volume 3 ¦ September 03, 2017